Diabetes is a chronic health condition that is one of the top causes of mortality and disability in the United States. According to the reports, over 34 million Americans get diagnosed with diabetes every year, and an additional 24 million individuals aged 65 and above are currently living with prediabetes. This long-term illness can put individuals at risk of additional health issues. A foot ulcer is one of the most common complications associated with uncontrolled diabetes, often resulting in osteomyelitis or bone infection, which can ultimately lead to the amputation of the lower extremities.
To address the foot-related issues associated with diabetes, consulting a podiatrist is crucial. In this blog post, we will share a detailed understanding of the role that podiatrists play in diabetes care, including the conditions they treat and how to find a good podiatrist. Read on to learn more.
Who is a Podiatrist?
A podiatrist is a healthcare professional specializing in diagnosis, treatment, and prevention of conditions related to the feet, ankles, and lower extremities. Also known as Doctors of Podiatric Medicine (DPMs), podiatrists have a comprehensive understanding of the intricate structure and biomechanics of the foot. It allows them to diagnose and treat conditions affecting an individual’s ability to walk, run, or perform daily activities comfortably.
Podiatrists play a crucial role in managing foot complications that can arise from diabetes. By conducting regular foot exams, providing preventive care, and addressing potential issues promptly, podiatrists help diabetic individuals avoid serious complications such as infections, ulcers, and amputations.
Why Foot Care is Important for Diabetic Individuals
Diabetes can damage nerves and reduce blood circulation in the feet, causing peripheral arterial disease. These conditions can decrease sensation in the feet, making it difficult for individuals to detect injuries, ulcers, or other foot deformities. Additionally, poor blood circulation slows down the healing process, making even minor cuts or blisters susceptible to infection and more severe complications.
Moreover, diabetes is one of the leading causes of non-traumatic lower limb amputations. If diabetic foot ulcers, injuries or blisters are left untreated or improperly managed for a long time, they can become infected. These infections can eventually lead to serious consequences, such as cellulitis, osteomyelitis, and in severe cases, amputation.
However, it is possible to reduce the risk of these complications with proper diabetic foot care and timely intervention.
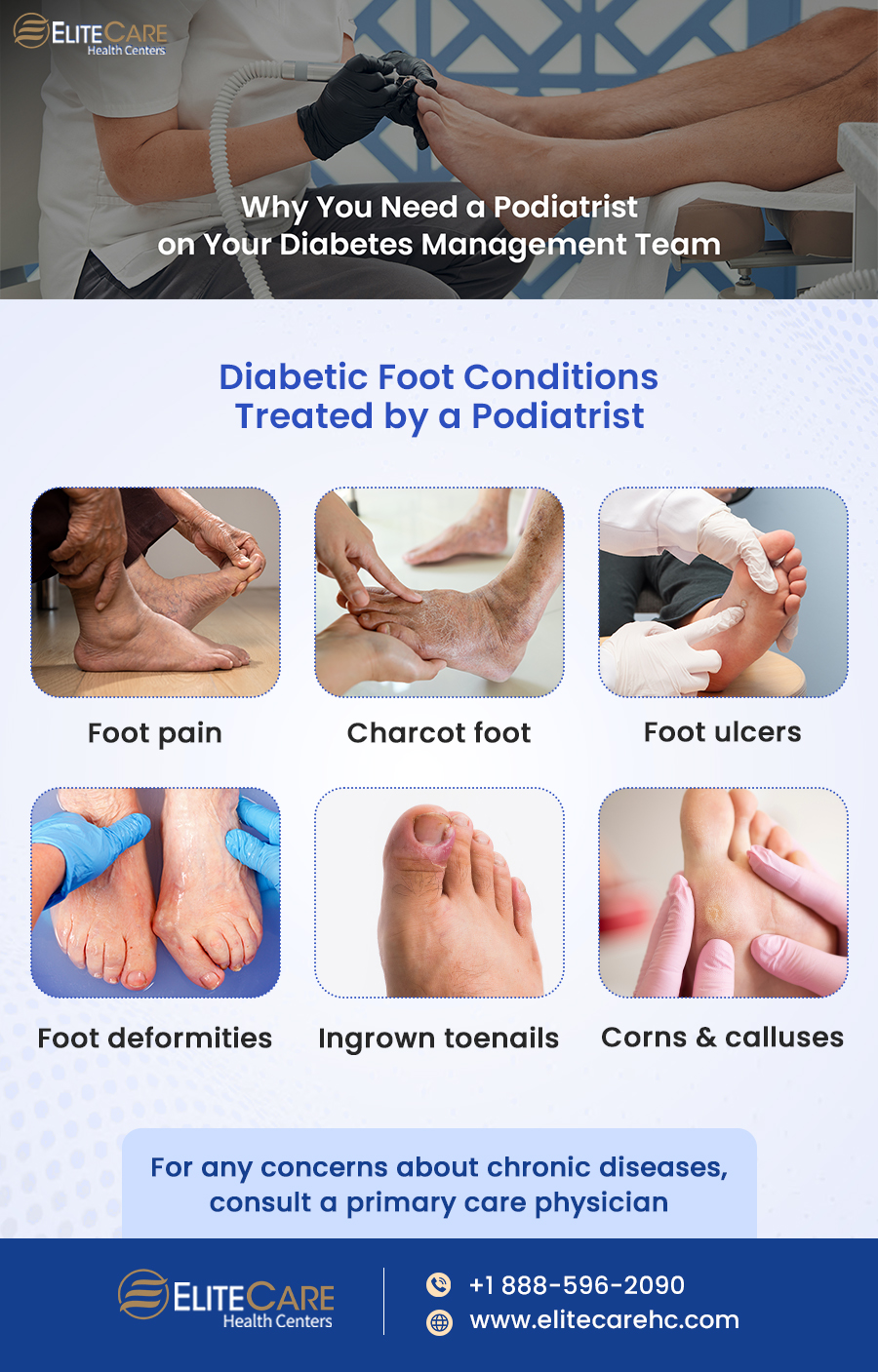
Diabetic Foot Conditions Treated by a Podiatrist
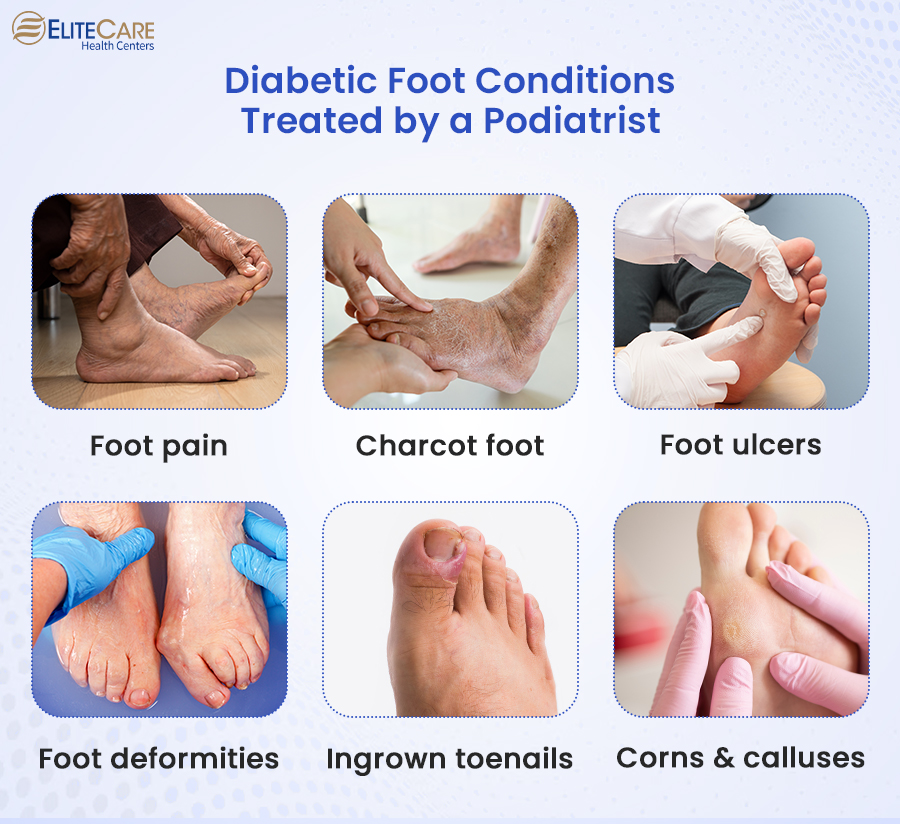
Foot pain
Diabetic neuropathy is a condition characterized by nerve damage caused by uncontrolled high blood sugar levels. This nerve damage can result in tingling, burning, or shooting pain in the feet and lower legs. Neuropathic foot pain may be present even without an obvious injury or cause.
A podiatrist may recommend orthotic devices, prescribe medications and provide guidance on foot protection techniques to manage foot pain effectively.
Charcot foot
It is a condition characterized by weakened bones and joint deformities due to nerve damage in the feet. Some form of trauma or injury to the foot is the primary cause of a Charcot foot. This trauma can be a result of repetitive stress, such as prolonged walking or standing, or a single traumatic event, like a fall or injury. Due to neuropathy, diabetic individuals may not feel pain associated with the trauma, leading to continued pressure and further damage to the foot.
Podiatrists can recommend immobilization, orthotic devices, and therapeutic shoes to support and protect the foot structure.
Diabetic foot ulcers
These types of open sores or wounds occur due to poor circulation and neuropathy. Diabetic foot ulcers commonly occur at the bottom of the foot or in areas where we put high pressure during walking or standing. They are often painless due to the loss of sensation caused by neuropathy, which can further delay their detection and prompt treatment.
Podiatrists are skilled in assessing and managing diabetic foot ulcers in the early stages. They can provide appropriate wound care and prescribe medications to promote healing and prevent infection.
Foot deformities
Diabetes can also lead to foot deformities, such as hammertoes, bunions, and claw toes, which can cause discomfort and difficulty with walking. Podiatrists can provide non-surgical interventions like splinting, padding, and custom orthotics to alleviate symptoms and improve foot function.
Podiatrists often recommend non-surgical interventions like splinting, padding, and custom orthotics to alleviate symptoms and improve foot function.
Ingrown toenails and corns/calluses
Ingrown toenails occur when the edge or corner of a toenail grows into the surrounding skin instead of over it. Diabetes can contribute to the development of ingrown toenails due to factors such as poor circulation, neuropathy (nerve damage), and altered foot structure. Similarly, diabetes can also cause corn and calluses, where the skin thickens in response to prolonged pressure or friction.
Podiatrists may perform nail avulsion or debridement to relieve pain and prevent complications related to ingrown toenails, corn and calluses.
How to Find a Good Podiatrist
- Seek recommendations from your primary care physician, family members, friends, or other healthcare professionals. Personal referrals can provide valuable insights into a podiatrist’s expertise and patient experience.
- Research credentials and qualifications to check whether the podiatrist is board-certified. Check their educational background, training, certifications, and affiliations with professional organizations.
- Check online reviews and ratings from reliable sources such as healthcare review websites or patient feedback platforms. These reviews can provide insights into the podiatrist’s reputation, patient satisfaction, and quality of care.
- Consider the podiatrist’s experience and specialization in diabetic foot care.
- Verify if the podiatrist accepts any health insurance plan, check coverage and any potential out-of-pocket expenses.
- Choose a podiatrist whose office is located nearby and offers flexible scheduling options and online doctor consultation facilities.
The frequency of visits to the podiatrist can vary depending on individual needs and foot health. While individuals with no specific foot concerns or chronic conditions can visit a podiatrist for routine foot care once a year, more frequent visits may be necessary for those with diabetes.
Medicare Coverage for Diabetic Foot Care
The Bottom Line
According to a CDC report, approximately 130,000 diabetes-related hospital discharges involve a lower-extremity amputation, mainly due to delayed diagnosis of foot-related issues. Whether it is about managing existing issues or preventing future complications – podiatrists provide comprehensive foot care for diabetic individuals. They work alongside primary care physicians, endocrinologists, vascular surgeons, and infectious disease specialists to provide multidisciplinary diabetes care.
For any queries or concerns related to diabetes-related foot care, contact EliteCare Health Centers, one of the best medical clinics in Florida, which offers a wide range of senior care services.