A chronic digestive disorder characterized by the frequent or persistent flow of stomach acid and other gastric content back into the esophagus, is known as Reflux Disorder or Gastroesophageal Reflux Disease (GERD).
The esophagus, a tube that connects the throat to the stomach, carries food and liquids from the mouth to the stomach. When the lower esophageal sphincter (LES), a ring of muscles located at the bottom of the esophagus, does not function properly, it allows the acidic content to reflux or regurgitate back into the esophagus.
GERD is a common condition that affects people of all ages, but it is more prevalent in adults, especially those over the age of 40. In this blog post, we will share detailed insights into GERD, its symptoms, and how to manage it. Read on to learn more.
Why Seniors Are at an Increased Risk for Gastroesophageal Reflux Disease (GERD)
1. Weakened muscles
Lower Esophageal Sphincter (LES), a ring of muscles situated at the bottom of the esophagus, works like a barrier and prevents stomach acid from flowing back up into the esophagus. As individuals age, the muscles that help keep the LES closed also weaken. Therefore, it increases the risk of acid reflux.
2. Hiatal hernias
Seniors are more prone to developing hiatal hernias, a condition in which a portion of the stomach extends beyond the diaphragm into the chest cavity. Hiatal hernias can disrupt the normal functioning of the LES, allowing stomach acid to reflux into the esophagus.
3. Reduced saliva production
Aging often leads to a decrease in saliva production which plays a crucial role in neutralizing stomach acid and protecting the esophagus. With reduced saliva production, seniors may experience acid reflux.
4. Medications
Older adults often take multiple medications since they suffer from multiple chronic health conditions. Some medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs), aspirin, muscle relaxants, and certain blood pressure medications, can increase the risk of GERD or exacerbate its symptoms.
5. Slower digestive system
With age, the pace of digestive functions slows down. This delay in the digestive process can contribute to acid reflux as food and stomach acids remain in the stomach for a longer duration, increasing the likelihood of reflux.
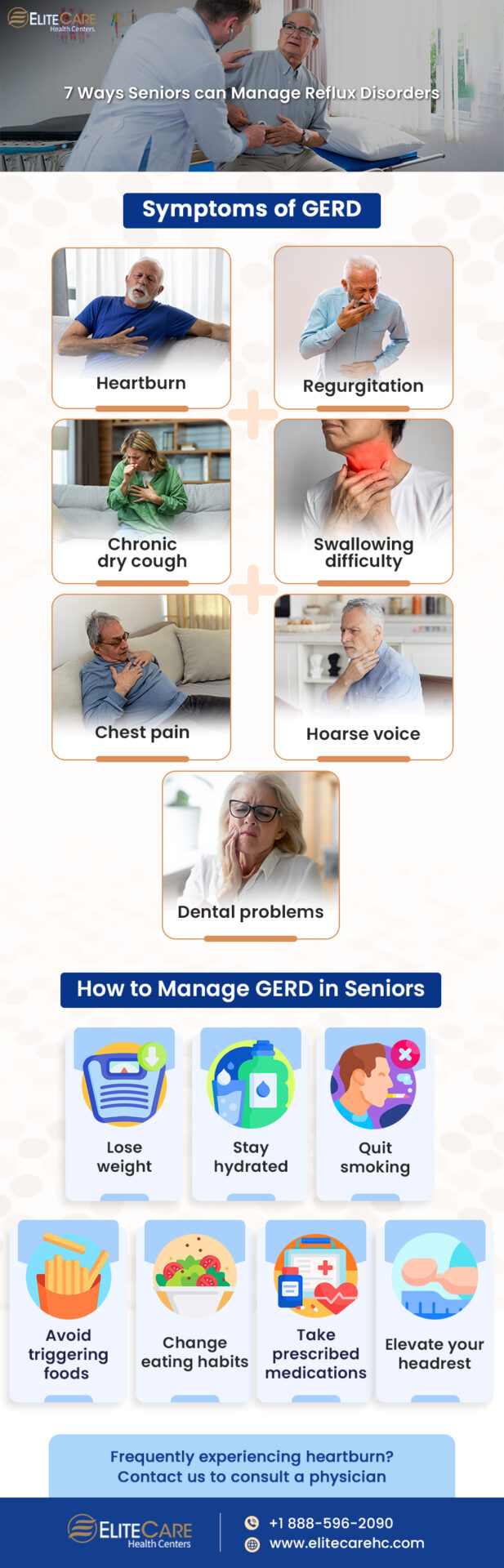
Symptoms of GERD in Seniors

Although symptoms of GERD can vary from person to person, there are some common signs which are as follows:
Heartburn
Burning sensation or discomfort in the chest, often experienced after eating, lying down, or bending over.
Regurgitation
Sour or bitter taste in the mouth when stomach acid or undigested food flows back into the throat or mouth.
Chest pain
Discomfort and tightness in the chest that can be mistaken for heart-related issues.
Dysphagia
Discomfort or difficulty while swallowing, often occurring due to inflammation or narrowing of the esophagus.
Chronic cough
Persistent dry cough that tends to worsen at night or after eating.
Hoarse voice
Irritation of the throat caused by stomach acid reflux, resulting in a hoarse voice or persistent sore throat.
Dental problems
Frequent exposure to stomach acid can lead to tooth enamel erosion, tooth sensitivity, cavities, or tooth decay.
Individuals experiencing any of these symptoms should visit a medical clinic and seek medical evaluation immediately for accurate diagnosis and appropriate treatment.
Read More: What to Expect During a Routine Dental Exam
How to Manage GERD in Seniors

Managing Gastroesophageal Reflux Disease (GERD) in seniors involves a comprehensive approach that includes lifestyle modifications, dietary changes, and, in some cases, medication. The following are some effective ways to manage this digestive disorder:
1. Lose weight
Excess weight can increase pressure on the abdomen and lower esophageal sphincter (LES), eventually contributing to acid reflux. Encouraging gradual weight loss through a balanced diet and regular physical activity can significantly help manage GERD symptoms.
In addition, obesity is also associated with chronic low-grade inflammation, which can worsen the symptoms of GERD. Maintaining a healthy weight can reduce the risk of inflammation in the esophagus, decreasing the frequency and intensity of GERD symptoms.
2. Avoid triggering foods
Certain foods and beverages can exacerbate GERD symptoms in seniors. While triggers can vary among individuals, common foods include:
- Spicy and fatty foods
- Citrus fruits and juices
- Tomatoes and tomato-based products
- Chocolate
- Beverages containing caffeine (coffee, tea)
- Alcohol
- Carbonated beverages
Older adults should consider adding more fiber to their diet to maintain regular bowel movements and prevent constipation. Avoiding constipation is a crucial part of managing GERD as it can contribute to increased pressure on the abdomen and worsen GERD symptoms.
3. Change eating habits
Seniors should limit their portion size and eat more frequent meals throughout the day to reduce the pressure on the stomach and decrease the likelihood of acid reflux. Additionally, practicing mindful eating can also help manage GERD symptoms. Take time to eat slowly and chew food thoroughly to encourage better digestion.
4. Drink adequate water
Drinking enough water throughout the day helps dilute stomach acid, therefore reducing the burning sensation and discomfort associated with acid reflux. In addition, adequate hydration can also help seniors digest food easily and keep the esophageal tissues hydrated. As a result, it protects the esophagus from inflammation, irritation and reduces the intensity of dysphagia.
5. Quit smoking
It is one of the most important parts of managing GERD symptoms because smoking damages the delicate lining of the esophagus and impairs its ability to heal. Chronic exposure to smoke can cause inflammation, irritation, and weakening of the esophageal tissues, making them more susceptible to damage from stomach acid.
Additionally, cigarettes can also stimulate the production of stomach acid, which can exacerbate GERD symptoms.
6. Take prescribed medications
Seniors should not miss medications prescribed by their healthcare provider to alleviate the symptoms. Proton Pump Inhibitors (PPIs), H2 Blockers, and antacids are the most commonly prescribed medications for GERD.
7. Elevate the head of the bed
Raising the head of the bed by using blocks or wedges can help prevent stomach acid from flowing back into the esophagus while sleeping. Seniors can also try using extra pillows to increase the height of the headrest, creating an inclined sleeping position.
Seniors should follow their healthcare provider’s instructions thoroughly regarding medication use or lifestyle modifications for managing GERD.
The Bottom Line
Seniors often ignore Gastroesophageal Reflux Disease (GERD) as a minor health issue. As a result, it often develops into more serious complications like esophagitis or chronic respiratory issues in the long run. Persistent symptoms, such as heartburn, regurgitation, and chronic cough, can interfere with daily activities, disrupt sleep, and cause discomfort or pain. Seniors must consult a primary care physician to develop an individualized plan.
For any questions or concerns about GERD in seniors, contact EliteCare Health Centers, one of the best medical clinics in Florida that offers a wide range of senior care services.